Laparoscopic Pyeloplasty
Laparoscopic pyeloplasty is a way to perform reconstructive surgery of a narrowing or scarring where the ureter (the tube that drains urine from the kidney to the bladder) attaches to the kidney through a minimally invasive procedure.
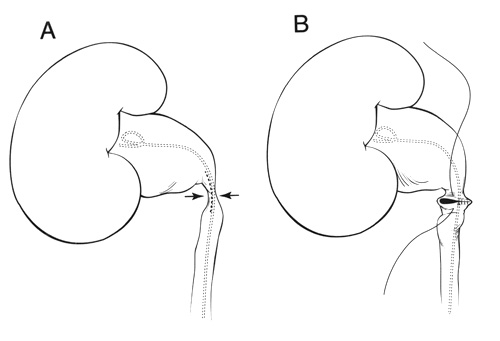
This operation is used to correct a blockage or narrowing of the ureter where it leaves the kidney. This abnormality is called a ureteropelvic junction (UPJ) obstruction which results in poor and sluggish drainage of urine from the kidney. UPJ obstruction can potentially cause abdominal and flank pain, stones, infection, high blood pressure and deterioration of kidney function.
When compared to the conventional open surgical technique, laparoscopic pyeloplasty has resulted in significantly less post-operative pain, a shorter hospital stay, earlier return to work and daily activities, a more favorable cosmetic result and outcomes identical to that of the open procedure.
The Surgery
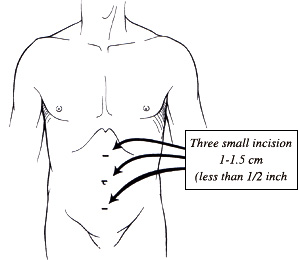
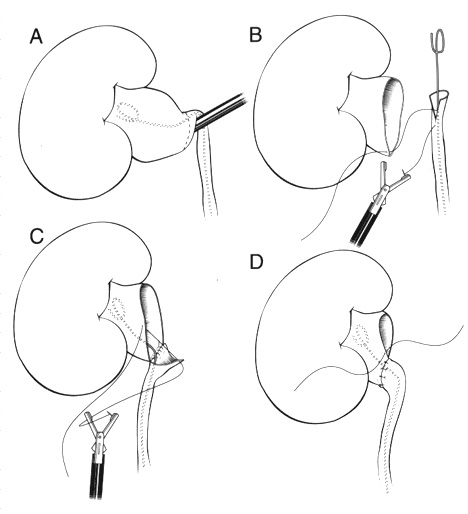
Laparoscopic pyeloplasty is performed under general anesthesia. The typical length of the operation is three to four hours. The surgery is performed through three small (1 cm) incisions made in the abdomen. A telescope and small instruments are inserted into the abdomen through these keyhole incisions, which allow the surgeon to repair the blockage/narrowing without having to place his or her hands into the abdomen.
A small plastic tube (called a ureteral stent) is left inside the ureter at the end of the procedure to bridge the pyeloplasty repair and help drain the kidney. This stent will remain in place for four weeks and is usually removed in the doctor’s office. A small drain will also be left exiting your flank to drain away any fluid around the kidney and pyeloplasty repair.
Potential Risks and Complications
Although this procedure has proven to be very safe, as in any surgical procedure there are risks and potential complications. The safety and complication rates are similar when compared to the open surgery. Potential risks include:
Bleeding: Blood loss during this procedure is typically minor (less than 100 cc) and a blood transfusion is rarely required. If you are still interested in autologous blood transfusion (donating your own blood) prior to your surgery, you must make your surgeon aware. When the packet of information is mailed or given to you regarding your surgery, you will receive an authorization form for you to take to the Red Cross in your area.
Infection: All patients are treated with broad-spectrum intravenous antibiotics prior to starting the surgery to decrease the chance of infection from occurring after surgery. If you develop any signs or symptoms of infection after the surgery (fever, drainage from your incision, urinary frequency, discomfort, pain or anything that you may be concerned about) please contact us at once.
Hernia: Hernias at incision sites rarely occur since all keyhole incisions are closed carefully at the completion of your surgery.
Tissue / organ injury: Although uncommon, possible injury to surrounding tissue and organs including bowel, vascular structures, spleen, liver, pancreas and gallbladder could require further surgery. Injury could occur to nerves or muscles related to positioning.
Conversion to open surgery: this surgical procedure may require conversion to the standard open operation if extreme difficulty is encountered during the laparoscopic procedure. This could result in a larger standard open incision and possibly a longer recuperation period.
Failure to correct UPJ obstruction: Roughly 3% of patients undergoing this operation will have persistent blockage due to recurrent scarring. If this occurs additional surgery may be necessary.
